Proper wound assessment is essential to prevent potential complications such as infection, necrosis, or abnormal healing. Traditionally, visual inspection has been the standard tool in hospitals and primary care centers. However, this approach has significant limitations: it depends heavily on the clinician’s experience, ambient lighting conditions, and the subjective interpretation of clinical signs.
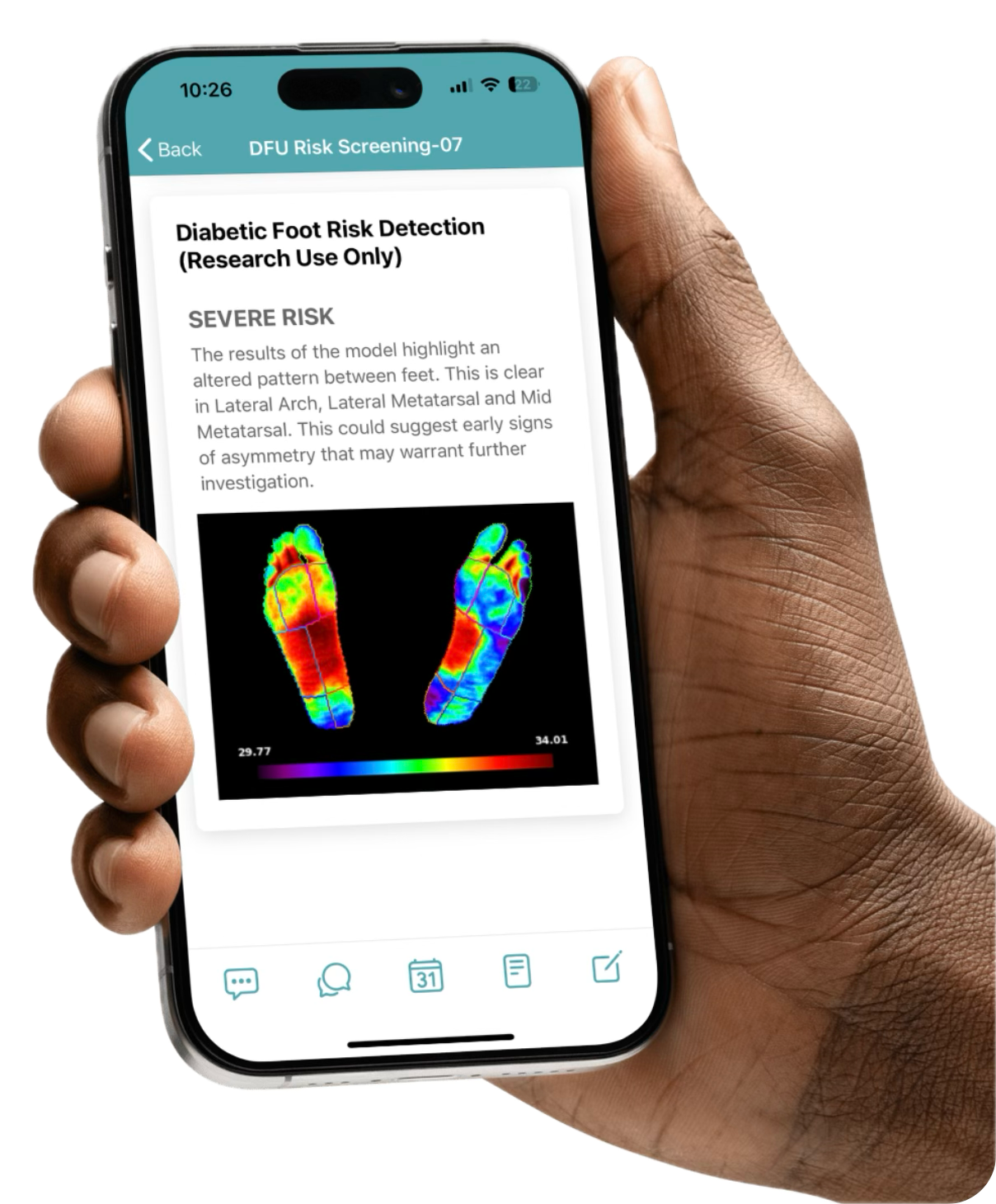
In response to these challenges, technologies like infrared thermography and artificial intelligence (AI) are becoming key tools to enhance diagnostic accuracy and anticipatory capabilities in wound management. In particular, the approach known as Spectral Intelligence—which integrates AI with clinical data and multiple imaging modalities, such as visible (RGB) and thermal imaging—is gaining increasing relevance in medical practice. Let’s explore its impact on clinical teams and the benefits these solutions bring to healthcare settings.
What Is Thermal Imaging and How Does It Work in Clinical Settings?
Thermal imaging is based on measuring the skin’s surface temperature using infrared cameras. In the context of wound care, this allows clinicians to detect thermal abnormalities associated with inflammation, infection, or ischemia — often before they become visible to the naked eye.
Recent studies have shown that:
- Infected areas can raise the local temperature by 1.5 °C to 3 °C compared to surrounding healthy tissue.
- Ischemic zones or those with poor perfusion tend to be colder, indicating a potential risk of necrosis.
Thanks to this technology, healthcare professionals can detect early signs of complications and take action before the wound deteriorates. Scientific literature clearly supports a correlation between temperature changes and signs of infection, highlighting the clinical value of thermal imaging in wound assessment.
Comparison: Visual vs. Thermal Assessment
| Criteria | Traditional Visual | Thermal with AI (e.g., Clinicgram) |
| Objectivity | Subjective and variable | Quantifiable and objective |
| Assessment time | Immediate, but operator-dependent | Fast, AI-automated |
| Predictive capacity | Limited (reactive) | High (proactive and preventive) |
| Requires contact | Often yes | No, contactless imaging |
| Longitudinal tracking | Photos or text-based | Thermal data with historical comparison |
This comparison highlights how thermography, especially when combined with AI, overcomes many limitations of traditional visual assessment.
Clinicgram’s Added Value in Thermal Wound Analysis
Clinicgram enhances thermography with artificial intelligence algorithms and computer vision, delivering added value and clinical benefits:
- Automatic interpretation of thermal maps: identifies thermal asymmetries and alerts clinicians to significant deviations.
- Structured documentation and traceability: each evaluation is stored with images, temperature values, and comparative data over time.
- Collaborative use: results can be shared across teams, enabling more coordinated and safer decision-making.
Moreover, since no physical contact is required, Clinicgram enables safe and hygienic wound assessment, even in infection control or home care settings.
Key benefits for Medical Teams and Patients
Once the clinical utility of this tool is clear, we can highlight its operational and clinical benefits:
- Complication reduction: various studies suggest that integrating thermography into the monitoring of pressure ulcers can significantly contribute to the reduction of infections.
- Improved clinical efficiency: helps prioritize interventions, optimize treatment plans, and reduce unnecessary hospital admissions.
- Empowers nursing staff: provides objective tools for decision-making without the need to escalate every case.
Real-World Applications: Clinical Use Cases
The value of thermal wound analysis goes beyond theory. Thanks to tools like Clinicgram, this technology is already part of daily clinical routines, transforming how teams monitor wound progression and make therapeutic decisions.
It’s no longer just about what we see, but about detecting what we can’t: visualizing invisible patterns, identifying thermal anomalies, anticipating infections, distinguishing inflammation from necrosis, or evaluating treatment effectiveness—all non-invasively, rapidly, and with full digital traceability.
Here are the main clinical scenarios where this technology has a proven and measurable impact:
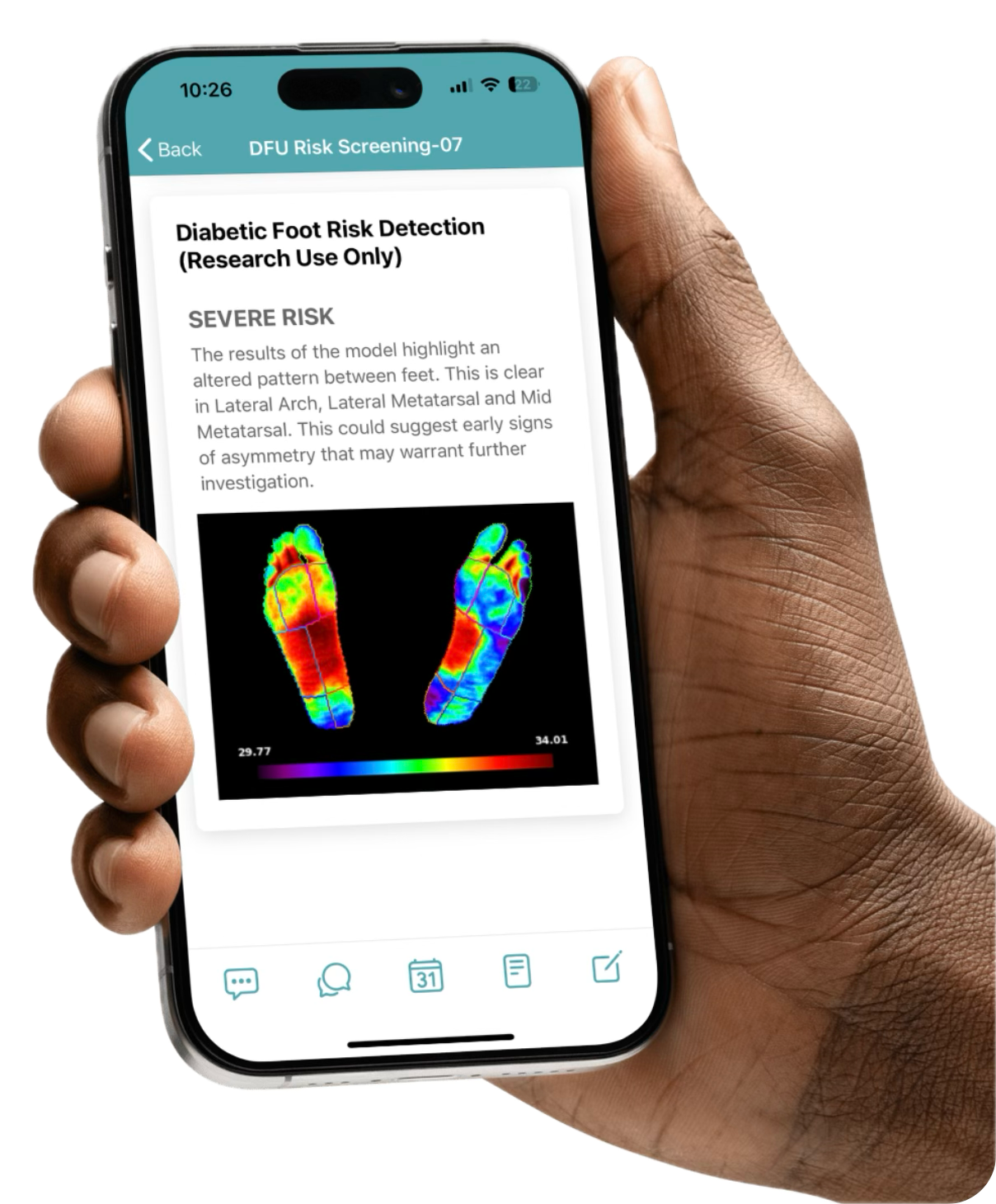
- Diabetic foot: identifies risk areas before visible ulceration develops.
- Pressure ulcers: daily contactless assessment, enabling early detection of infection or necrosis.
- Surgical wounds: post-operative monitoring to reduce the risk of surgical site infections (SSIs).
Additionally, its use in telemedicine and home healthcare makes it especially valuable in rural settings or regions with high care demand and limited access.
Conclusion: Toward a More Accurate and Preventive Clinical Approach
The combination of thermal imaging, artificial intelligence, and clinical digitalization is revolutionizing wound management. With solutions like Clinicgram, healthcare teams are moving toward a more objective, predictive, and collaborative care model—significantly improving patient outcomes and the quality of care.

Ready to Elevate Your Wound Care Practice? Clinical wound evaluation is evolving. If you’re looking to take your practice to the next level, Clinicgram is your technological partner. Request a personalized demo today and start transforming the way you assess and manage wounds. Contact our team.
Please rate this post