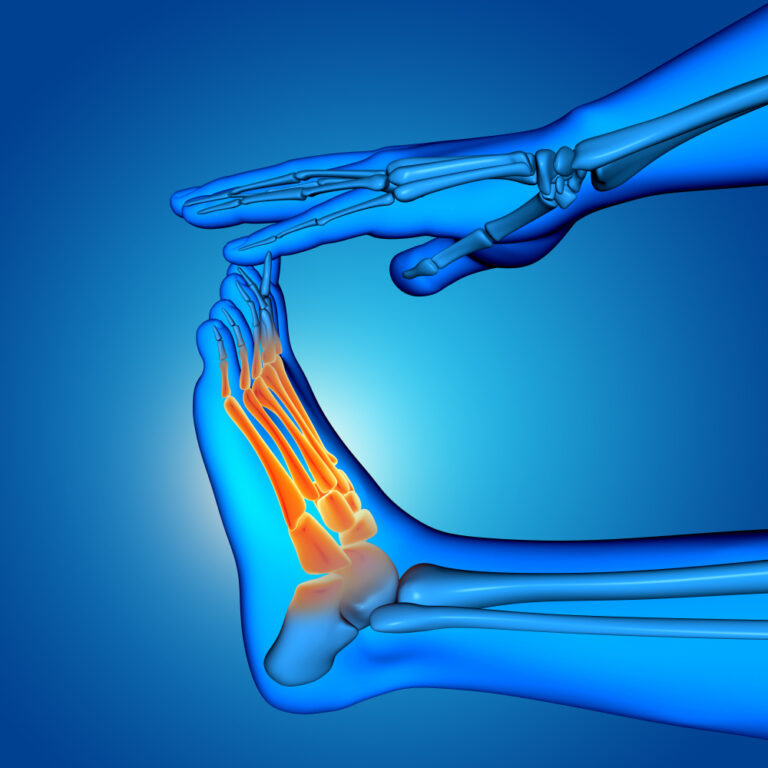
Diabetic foot is one of the most serious and costly complications of diabetes mellitus. It is estimated that up to 34% of people with diabetes will develop a foot ulcer during their lifetime, and approximately 20% of these cases will require hospitalization. These lesions not only increase the risk of amputation, but also have a severe impact on quality of life and place a significant burden on healthcare systems.
Prevention and early diagnosis are essential to avoid severe outcomes. However, traditional approaches to diabetic foot care often fall short in terms of objectivity, continuity, and predictive capacity. In this context, digital technologies have emerged as essential tools to improve wound management and clinical outcomes.
Common complications in diabetic foot
The most frequent complications associated with diabetic foot include infections, ulcerations, and, in advanced cases, limb amputations. Diabetic foot ulcers (DFUs) are associated with high morbidity and mortality. Around 5% of patients with DFUs require lower-limb amputation, and the five-year mortality rate is comparable to that of several major cancers.
In addition, DFUs are linked to a significant loss of mobility, increased anxiety and depression, and a considerable economic burden on healthcare systems. In the United States, the annual costs associated with diabetic foot complications exceed $11.7 billion.
Limitations of traditional care
The conventional approach to managing diabetic foot includes periodic visual inspection, palpation of peripheral pulses, and sensitivity testing. However, these methods are subjective and highly dependent on the healthcare provider’s experience. Moreover, many patients struggle to perform reliable self-examinations due to physical or cognitive limitations.
The lack of objective and continuous monitoring tools limits the ability to detect subtle changes that could indicate the onset of complications, leading to delayed interventions and increased risk of severe tissue damage.
Thermography and AI: allies in anticipating complications
Infrared thermography is a non-invasive technique that measures skin surface temperature, helping identify areas of inflammation or ischemia before they are clinically evident. Research shows that infected tissue can present local temperature increases of 1.5 °C to 3 °C compared to healthy surrounding areas.
Combining thermography with AI algorithms enables:
- Automatic detection of thermal anomalies: Identifying high-risk zones without manual interpretation.
- Longitudinal tracking: Comparing thermal images over time to assess lesion evolution.
- Early alerts: Proactively notifying clinicians of significant changes.
This combination significantly improves the ability to anticipate complications and enables timely clinical interventions.
The role of digital technologies in prevention
Preventing complications in diabetic foot requires innovative digital tools that enhance continuity, objectivity, and efficiency in clinical monitoring. Solutions like Clinicgram are revolutionizing traditional workflows by offering a platform that integrates artificial intelligence, thermal imaging, digital traceability, and real-time collaboration among care teams.
With Clinicgram, healthcare providers can benefit from:
- Structured, data-driven follow-up: The platform records, organizes, and visualizes the progression of diabetic foot lesions, supporting longitudinal, proactive care.
- Remote access and decentralized care: Designed for use in both clinical and home settings, Clinicgram is particularly effective in rural or high-demand environments or with patients with reduced mobility.
- Clinical decision support: By combining thermal imaging and AI analysis, the platform offers early alerts and highlights thermal asymmetries that may go unnoticed in visual assessments.
- Enhanced multidisciplinary communication: Clinical data and captured images can be easily shared between nurses, podiatrists, endocrinologists, and primary care physicians, improving coordination and continuity of care.
This type of digital solution shifts the model from reactive to predictive care, enabling early interventions, reducing hospitalizations, and preventing severe complications. Clinicgram not only delivers advanced tools, but also adapts to daily clinical workflows, enhancing both system efficiency and patient experience.
| Criterion | Conventional Strategy | With Clinicgram Technology |
| Assessment objectivity | Subjective, reliant on clinician’s experience | Quantifiable, based on thermal data and AI |
| Early detection of complications | Limited to advanced visual signs | Early identification of thermal anomalies before clinical symptoms appear |
| Clinical follow-up | Sporadic and manual (notes, unstructured photos) | Longitudinal, structured, and digital follow-up |
| Remote accessibility | Difficult or not available | Enabled for home care and rural settings |
| Clinical decision-making | Based on observation and practitioner judgment | AI-assisted with automatic alerts |
| Professional collaboration | Limited to written reports or calls | Instant sharing of data and images across multidisciplinary teams |
| Response time to changes | Depends on in-person visits | Proactive response enabled by continuous monitoring |
Real-world applications: technology in clinical practice
The implementation of digital technologies in diabetic foot care has proven effective across multiple clinical scenarios. Below are key contexts where these tools are being used successfully:
- Home care: Remote monitoring devices allow patients to receive continuous assessment without traveling to healthcare centers.
- Hospital-based specialized units: The integration of thermography and AI enables rapid and accurate lesion evaluation, optimizing clinical resources and improving patient outcomes.
- Telemedicine: Digital platforms facilitate virtual consultations, reducing geographic barriers and enhancing access to specialized care.
These use cases demonstrate the transformative potential of digital technologies in the management of diabetic foot.
Conclusion: toward proactive and digital diabetic foot management
The integration of digital technologies in diabetic foot management marks a major step forward toward more proactive, personalized, and efficient care. Tools such as thermography, AI, and remote monitoring platforms enable early detection of complications, reduce the progression to severe lesions, and improve patients’ quality of life.

Clinicgram is positioned as a strategic partner in this transformation, offering innovative solutions that support prevention, diagnosis, and longitudinal tracking of diabetic foot conditions. By embracing these technologies, healthcare professionals can optimize their clinical workflows and deliver more effective, patient-centered care.
Please rate this post